If you’ve been experiencing hand numbness, tingling fingers, or wrist pain, your doctor might immediately suspect carpal tunnel syndrome. But here’s what most people don’t know: several other conditions produce nearly identical symptoms, leading to misdiagnosis rates that affect thousands of patients every year.
Getting the wrong diagnosis means months of ineffective treatment, unnecessary surgery, and continued suffering. Let’s explore two conditions that doctors frequently confuse with carpal tunnel syndrome and how to tell the difference.
Understand Carpal Tunnel Syndrome First
Carpal tunnel syndrome occurs when the median nerve gets compressed as it passes through the carpal tunnel in your wrist. This creates numbness and tingling in your thumb, index finger, middle finger, and half of your ring finger. Your pinky finger stays unaffected because it’s connected to a different nerve.
The condition typically worsens at night, and many people report dropping objects or experiencing weakness in their grip. About 3-6% of adults in the United States experience carpal tunnel syndrome, making it one of the most common nerve compression disorders.
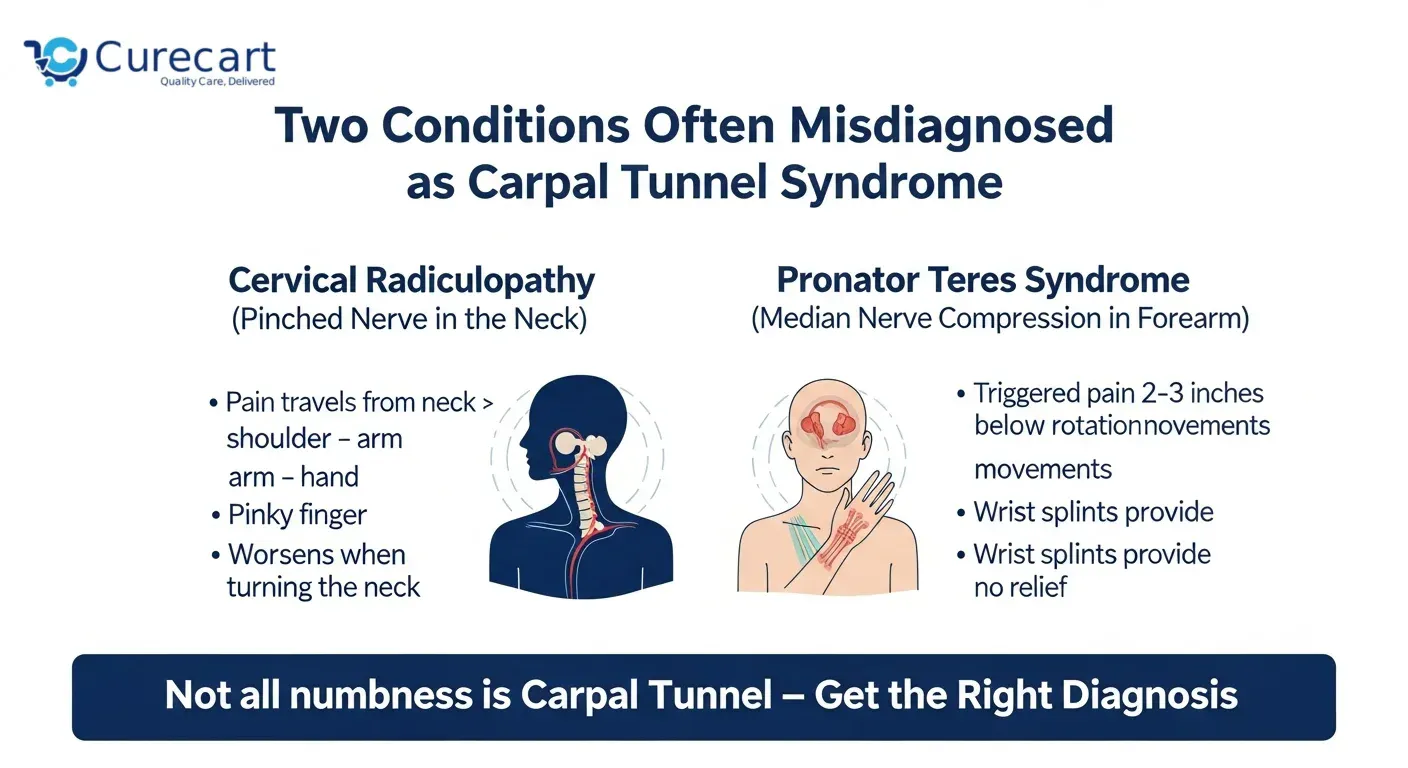
Cervical Radiculopathy (Pinched Nerve in the Neck)
Cervical radiculopathy happens when a nerve root in your neck becomes compressed or irritated. This compression sends pain, numbness, and tingling down your arm into your hand symptoms that mirror carpal tunnel syndrome almost perfectly.
The confusion makes sense. Both conditions involve nerve compression, both cause hand numbness, and both can make your fingers tingle. But the source of the problem sits in completely different locations.
Why the Misdiagnosis Happens:
When you complain about hand numbness, doctors often focus on your hand and wrist. They might not thoroughly examine your neck, especially if you don’t mention neck pain. Many people with cervical radiculopathy don’t even realize their neck is involved because the hand symptoms feel so prominent.
Research published in the Journal of the American Academy of Orthopaedic Surgeons found that cervical radiculopathy affects approximately 85 per 100,000 adults annually. The C6 and C7 nerve roots are most commonly affected, and these particular nerves send signals down to your hand and fingers.
Key Differences to Watch For:
Location of symptoms: Cervical radiculopathy typically affects your entire arm, not just your hand. You might feel pain in your shoulder, upper arm, forearm, and hand. Carpal tunnel syndrome stays localized to your wrist and specific fingers.
Pinky finger involvement: If your pinky finger feels numb or tingly, you’re dealing with cervical radiculopathy, not carpal tunnel syndrome. The median nerve doesn’t control your pinky.
Neck movement matters: Try turning your head or tilting it backward. If this reproduces or worsens your hand symptoms, your neck is likely the culprit. This is called Spurling’s test, and it’s a reliable indicator of cervical radiculopathy.
Pain patterns: Cervical radiculopathy often creates sharp, shooting pains that travel down your arm. Carpal tunnel syndrome produces more of a burning sensation or aching confined to the wrist and hand.
Night symptoms: Both conditions can worsen at night, but cervical radiculopathy symptoms often improve when you change your sleeping position or adjust your pillow. Carpal tunnel syndrome typically requires shaking out your hands for relief.
What Happens If You Get the Wrong Treatment:
If you receive carpal tunnel treatment for what’s actually cervical radiculopathy, you won’t improve. Some patients undergo unnecessary carpal tunnel release surgery, only to find their symptoms persist because the real problem remains in their neck.
The treatment approaches differ significantly. Cervical radiculopathy often responds to physical therapy focused on neck posture, specific exercises, and sometimes epidural steroid injections. Carpal tunnel syndrome benefits from wrist splinting, activity modification, and potentially carpal tunnel release surgery.
Pronator Teres Syndrome

Pronator teres syndrome involves compression of the median nerve the same nerve affected by carpal tunnel syndrome but at a different location. Instead of compression at the wrist, the nerve gets squeezed in your forearm by the pronator teres muscle.
This condition is significantly less common than carpal tunnel syndrome, which partially explains why it gets overlooked. Many healthcare providers simply aren’t as familiar with it.
Why the Misdiagnosis Happens So Often
Both conditions affect the median nerve, producing numbness in the same fingers: thumb, index, middle, and half of the ring finger. Both can cause weakness and difficulty with grip. The symptom overlap is substantial.
Doctors typically perform nerve conduction studies to diagnose carpal tunnel syndrome. However, these tests sometimes show abnormalities at the wrist even when pronator teres syndrome is the primary problem, leading clinicians down the wrong diagnostic path.
Pain location: Pronator teres syndrome creates pain in your forearm, particularly on the palm side about 2-3 inches below your elbow. Carpal tunnel syndrome centers pain around your wrist.
Specific movement triggers: Try this test: resist someone trying to turn your palm downward while your elbow is straight. If this reproduces your symptoms, pronator teres syndrome becomes more likely. This motion directly stresses the pronator teres muscle.
Tinel’s sign location: When a doctor taps along your nerve, both conditions can produce a tingling sensation. But in pronator teres syndrome, this happens in your forearm. In carpal tunnel syndrome, it happens at your wrist.
Forearm heaviness: People with pronator teres syndrome often describe a heavy, achy feeling in their forearm that worsens with repetitive palm-up, palm-down motions. This isn’t a typical carpal tunnel complaint.
Response to wrist splinting: If you’ve tried wearing a wrist splint at night and noticed zero improvement, pronator teres syndrome might be your actual diagnosis. Wrist splints don’t address forearm nerve compression.
Activities That Make It Worse
Pronator teres syndrome particularly affects people who perform repetitive gripping with their palm facing down. This includes activities like using a screwdriver, playing tennis with poor form, rock climbing, or working on an assembly line.
Computer work can aggravate both conditions, but pronator teres syndrome worsens specifically during mouse use and typing when your forearm muscles are actively engaged. Carpal tunnel syndrome often bothers you more during extended wrist flexion or extension.
The Treatment Mistake
Patients with undiagnosed pronator teres syndrome sometimes undergo carpal tunnel release surgery. The surgery might provide temporary relief because post-surgical swelling reduces overall nerve compression, but symptoms typically return once healing completes.
Proper treatment for pronator teres syndrome involves physical therapy to release the pronator teres muscle, activity modification, and sometimes surgery to decompress the nerve in the forearm a completely different procedure from carpal tunnel release.
How to Get the Right Diagnosis
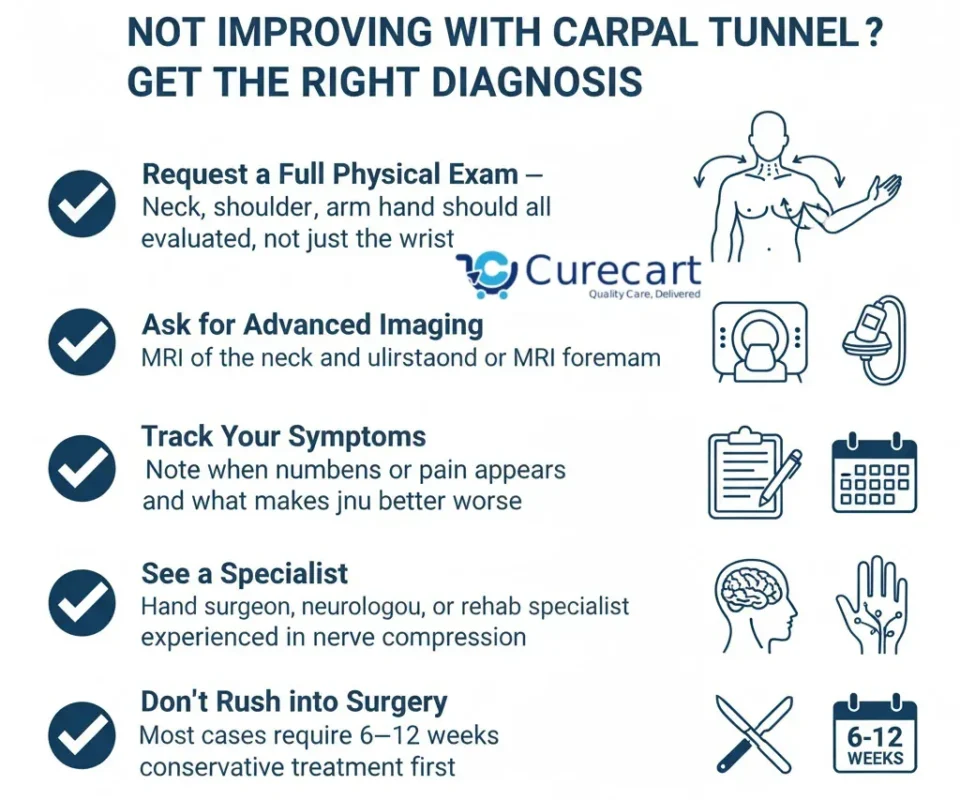
If you’ve been diagnosed with carpal tunnel syndrome but treatment isn’t working, push for a more comprehensive evaluation.
Request a thorough physical examination: Your healthcare provider should examine your neck, shoulder, entire arm, and hand—not just your wrist. They should perform specific tests for cervical radiculopathy and pronator teres syndrome.
Consider advanced imaging: While nerve conduction studies help, they don’t always tell the complete story. MRI of the cervical spine can reveal nerve compression in your neck. MRI or ultrasound of your forearm can show pronator teres muscle abnormalities.
Track your symptom patterns: Keep a detailed diary noting when symptoms occur, what makes them better or worse, and exactly where you feel pain, numbness, or tingling. This information helps clinicians distinguish between conditions.
Seek a specialist: If your primary care doctor or general orthopedist isn’t providing answers, consider seeing a hand surgeon, neurologist, or physical medicine and rehabilitation specialist who deals with nerve compression issues regularly.
Don’t rush into surgery: Unless you’re experiencing severe muscle wasting or complete loss of sensation, nerve compression conditions usually warrant trying conservative treatment for at least 6-12 weeks before considering surgery.
Why Accurate Diagnosis Matters
The difference between these conditions isn’t academic it directly affects your treatment and recovery. Carpal tunnel release surgery has excellent success rates when carpal tunnel syndrome is truly the problem. But performing this surgery on someone with cervical radiculopathy or pronator teres syndrome wastes time, money, and exposes you to surgical risks without addressing your actual condition.
Conservative treatments also differ significantly. Wrist splints help carpal tunnel syndrome but do nothing for cervical radiculopathy. Neck exercises benefit cervical radiculopathy but won’t help carpal tunnel syndrome. Forearm muscle release techniques work for pronator teres syndrome but are irrelevant for the other two conditions.
Final Thought
Hand numbness and tingling deserve proper investigation. If you’re not improving with carpal tunnel treatment, don’t accept “give it more time” as an answer. Your symptoms might be coming from your neck or forearm, not your wrist. Your hands are too important to settle for guesswork. Demand diagnostic precision, and don’t stop until you get answers that lead to real improvement.
References:
- Caridi, J. M., Pumberger, M., & Hughes, A. P. (2011). Cervical radiculopathy: a review. HSS Journal, 7(3), 265-272.
- Rodner, C. M., Tinsley, B. A., & O’Malley, M. P. (2013). Pronator syndrome and anterior interosseous nerve syndrome. Journal of the American Academy of Orthopaedic Surgeons, 21(5), 268-275.
- Atroshi, I., Gummesson, C., Johnsson, R., Ornstein, E., Ranstam, J., & Rosén, I. (1999). Prevalence of carpal tunnel syndrome in a general population. JAMA, 282(2), 153-158.