Elevated alkaline phosphatase (ALP) levels can be a concerning finding on blood tests, often indicating potential issues with the liver, bones, or other systems. ALP is an enzyme found throughout the body, with higher concentrations in the liver, bile ducts, bones, kidneys, and intestines. Its primary role involves breaking down proteins and facilitating processes like bone mineralization and bile acid management. Normal ALP levels for adults typically range from 30 to 130 international units per liter (IU/L), but this can vary based on age, sex, and lab standards children and pregnant individuals naturally have higher levels due to growth and placental activity. When ALP exceeds the upper limit, it doesn’t always signal disease, but persistent elevations warrant investigation to rule out serious conditions.
Key Foods to Avoid and Why
Based on evidence, the following foods can worsen conditions linked to high ALP. Avoidance is particularly crucial for liver causes, which predominate in adults. Portions and frequency matter; moderation may suffice for mild cases, but strict limits are advised for confirmed liver or bone issues.
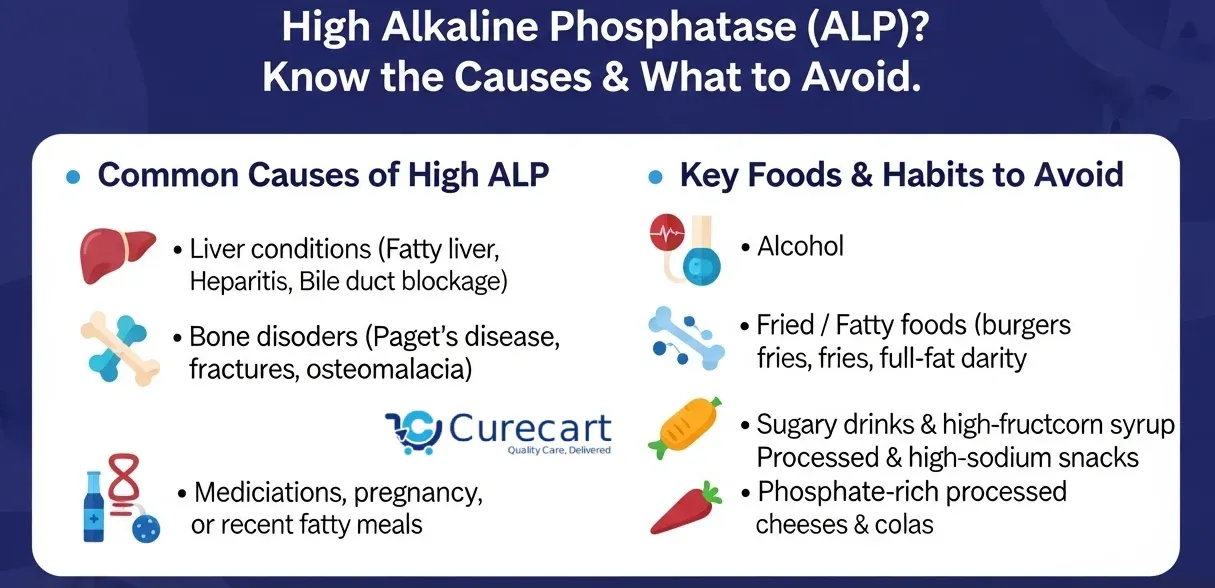
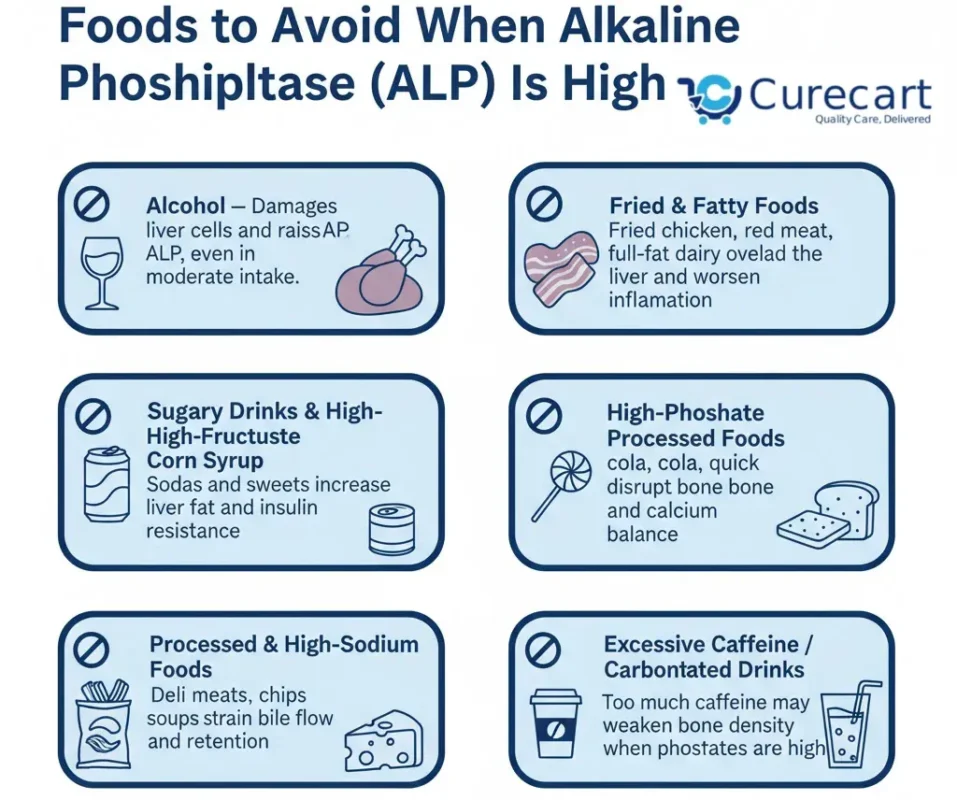
Alcohol
Alcohol is a top offender, directly damaging liver cells and promoting fatty buildup, which elevates ALP in conditions like alcoholic hepatitis or cirrhosis. Even moderate consumption can irritate bile ducts, worsening obstructions. Studies link chronic alcohol use to sustained enzyme spikes, and abstinence is key for recovery.
Fried and Fatty Foods
High-fat items like fried chicken, French fries, fatty red meats, and full-fat dairy overload the liver, aggravating NAFLD and cholestasis common ALP elevators. Saturated fats increase inflammation and triglyceride accumulation, straining hepatic function. Animal models show high-fat diets elevate ALP, ALT, and AST, while fiber-enriched variants reverse this (The beneficial impact of plant-based fiber-enriched diets on hepatic enzymes in streptozotocin-induced diabetic rats, Future Foods, 2023). Opt for lean proteins and plant-based fats instead.
Sugary Drinks and High-Fructose Corn Syrup
Sodas, candies, and processed sweets with high-fructose corn syrup spike insulin resistance and liver fat, fueling NAFLD. A 2020 animal study noted high-fructose diets increase ALP via oxidative stress. These also contribute to obesity, a risk factor for metabolic ALP elevations.
Processed and High-Sodium Foods
Canned soups, deli meats, chips, and ultra-processed snacks retain fluid, strain bile flow, and add preservatives that burden the liver. High sodium exacerbates edema in liver disease, indirectly raising ALP. Cross-sectional data show ultra-processed intake correlates with fatty liver and enzyme abnormalities.
High Phosphate Processed Foods
If ALP stems from bone turnover (e.g., Paget’s disease), limit phosphate additives in colas, processed cheeses, and quick breads. Excess phosphates can disrupt calcium balance, complicating remodeling. Natural dairy is generally fine in moderation, but check labels for additives.
Excessive Caffeine and Carbonated Drinks
While moderate coffee may lower ALP (a 2012 study found lower levels in current drinkers), excess caffeine or sodas can leach bone minerals if phosphates are high, potentially worsening bone-related elevations.
Additional Considerations
Avoid excessive vitamin A from supplements or organ meats like liver, as high doses stress bones. Smoking, though not a food, amplifies risks and should be quit. For low ALP (opposite issue), zinc- and magnesium-rich foods raise levels, but that’s irrelevant here (Low Alkaline Phosphatase (ALP) In Adult Population an Indicator of Zinc (Zn) and Magnesium (Mg) Deficiency, diet and nutrition Sciences, 2017).
Foods to Include for Support
To counterbalance, incorporate ALP-friendly options: leafy greens, oats, soy, fruits, and veggies for phytochemicals and fiber. Zinc sources like oysters or nuts support if deficiency contributes, but excess can raise ALP if already high (Do Certain Foods Raise Alkaline Phosphatase Levels?, Livestrong.com, 2019). Aim for balanced meals to aid detoxification and bone health.
The focus here is on foods to avoid, backed by evidence from authoritative sources, alongside supportive lifestyle tips. Remember, dietary adjustments should complement medical advice, not replace it consult a healthcare provider for personalized guidance, especially if symptoms like fatigue, jaundice, or bone pain are present.
What Causes High Alkaline Phosphatase Levels?
High ALP often stems from liver or bone-related issues, though other factors can contribute. Liver conditions account for many cases, as the enzyme leaks into the bloodstream when hepatocytes are damaged or bile flow is obstructed. Common liver causes include non-alcoholic fatty liver disease (NAFLD), hepatitis, cirrhosis, and bile duct blockages like gallstones or primary biliary cholangitis. Bone-related elevations occur with increased osteoblast activity, seen in Paget’s disease, osteomalacia, fractures, or certain cancers like osteogenic sarcoma.
Other contributors include pregnancy (placental ALP), medications (e.g., antibiotics or anticonvulsants), and even temporary factors like a recent fatty meal, which can mildly elevate levels in people with blood types O or B (Alkaline Phosphatase, StatPearls – NCBI Bookshelf, 2023). Genetic factors play a role too; for instance, low intestinal ALP has been linked to higher diabetes risk, suggesting protective effects of the enzyme against metabolic issues (A High Level of Intestinal Alkaline Phosphatase Is Protective Against Type 2 Diabetes Mellitus Irrespective of Obesity, EBioMedicine, 2015). Diagnostic approaches involve fractionating ALP isoenzymes to pinpoint the source, alongside tests like gamma-glutamyl transferase (GGT) for liver specificity or imaging for bone assessment (Diagnostic Approach to Abnormal Alkaline Phosphatase Value, Mayo Clinic Proceedings, 2025).
Symptoms vary by cause: liver issues may present with jaundice, abdominal pain, or dark urine, while bone problems could involve pain, deformities, or fractures. Risk factors include obesity, alcohol use, viral infections, and nutrient imbalances. Notably, a study of over 15,000 adults found that higher serum ALP correlates with increased all-cause and cardiovascular mortality, underscoring the need for prompt management (Associations of serum alkaline phosphatase level with all-cause and cardiovascular mortality: The National Health and Nutrition Examination Survey 1999–2016, Frontiers in Endocrinology, 2023).
The Role of Diet in Managing High ALP
Diet doesn’t directly lower ALP but supports the organs involved, potentially stabilizing or reducing levels over time. For liver-dominant elevations, anti-inflammatory, low-fat diets reduce strain and inflammation. Research indicates that high-calorie, high-carbohydrate diets can slightly increase ALP activity by 6% compared to balanced ones, highlighting the impact of caloric excess (The influence of diet upon liver function tests and serum lipids in healthy male volunteers resident in a Phase I unit, British Journal of Clinical Pharmacology, 2004). Conversely, plant-based, fiber-rich diets lower hepatic enzymes, including ALP, in models of diabetes and fatty liver (The beneficial impact of plant-based fiber-enriched diets on hepatic enzymes in streptozotocin-induced diabetic rats, Future Foods, 2023).
Higher intake of phytochemicals from fruits and vegetables is inversely associated with liver ALP, suggesting protective effects against elevations (Dietary phytochemical consumption is inversely associated with liver alkaline phosphatase in Middle Eastern adults, PLoS One, 2022). For bone-related highs, avoiding excess phosphates or vitamin A helps maintain mineral balance, though evidence is less direct. Overall, a Mediterranean-style diet emphasizing whole foods shows promise in supporting liver health and normalizing enzymes.
Tips Beyond Diet

- Weight Management: Losing 5-10% body weight improves fatty liver markers and ALP.
- Exercise: Regular activity reduces liver fat; aim for 150 minutes weekly.
- Hydration: Adequate water supports bile flow.
- Monitoring: Retest ALP every 3-6 months; track with apps.
- Medications: Review with a doctor, as some raise ALP.
- When to Seek Help: Persistent highs (>1.5x normal) or symptoms require specialist input, like a hepatologist.
In summary, managing high ALP involves targeting the cause through diet, with avoidance of alcohol, fats, sugars, and processed items as priorities. Evidence supports these changes for liver and bone health, but they’re most effective alongside medical care.
References:
- What Foods To Avoid If Alkaline Phosphatase Is High – Nourish (2024).
- Alkaline Phosphatase (ALP): Tests and Results – WebMD (2025).
- Dietary phytochemical consumption is inversely associated with liver alkaline phosphatase in Middle Eastern adults – PLoS One (2022).
- The influence of diet upon liver function tests and serum lipids in healthy male volunteers resident in a Phase I unit – British Journal of Clinical Pharmacology (2004).
- Low Alkaline Phosphatase (ALP) In Adult Population an Indicator of Zinc (Zn) and Magnesium (Mg) Deficiency – Food and Nutrition Sciences (2017).
- Alkaline Phosphatase (ALP) blood test – Mayo Clinic (2025).
- A High Level of Intestinal Alkaline Phosphatase Is Protective Against Type 2 Diabetes Mellitus Irrespective of Obesity – EBioMedicine (2015).
- Diagnostic Approach to Abnormal Alkaline Phosphatase Value – Mayo Clinic Proceedings (2025).
- Foods That Lower Alkaline Phosphatase – Everyday Health.
- Associations of serum alkaline phosphatase level with all-cause and cardiovascular mortality: The National Health and Nutrition Examination Survey 1999–2016 – Frontiers in Endocrinology (2023).
- The beneficial impact of plant-based fiber-enriched diets on hepatic enzymes in streptozotocin-induced diabetic rats – Future Foods (2023).
- Alkaline Phosphatase – StatPearls – NCBI Bookshelf (2023).
- Alkaline Phosphatase: MedlinePlus Medical Test.